Infection after a knee replacement is a devastating complication. We recently published an article using data over a 15-year period following patients with these infections. Many patients required further major operations before the infection was treated.
https://www.thieme-connect.de/products/ejournals/abstract/10.1055/a-2337-2402
There are many different types of bacteria that can lead to infection, with one of the main sources coming from the primary operation.
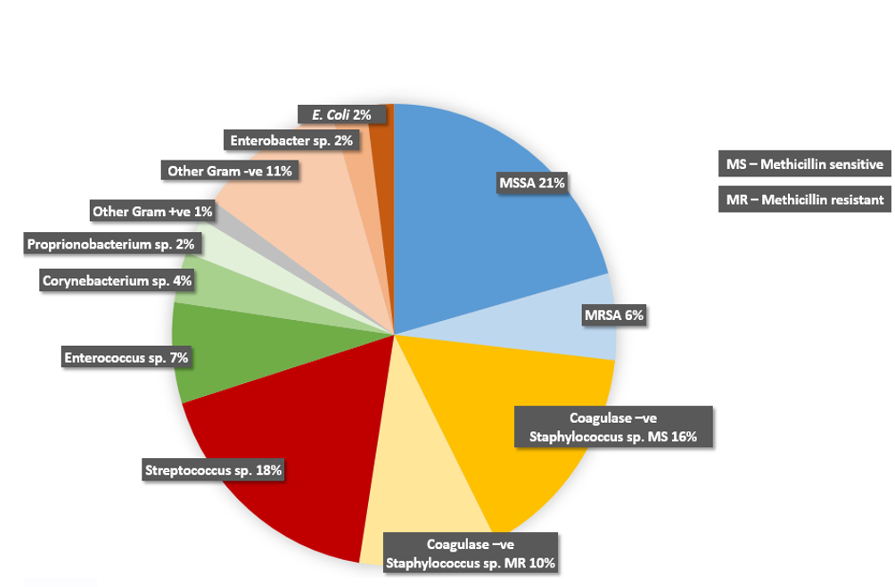
Bacteria live on our skin and are on every surface we touch. Careful regulation of airflow in theatre and the use of sterile drapes and instruments aren’t enough to prevent infection.
Here I lay out my protocol for a knee replacement in Bristol. This reduces the risk of periprosthetic infection to the minimum, and the lowest rate in the UK:
Pre-op planning
- Skin swabs are taken looking for resistant bacteria
- Underlying infections in other body areas need to be diagnosed and treated
- Cuts or breaks in the skin of the leg need to be healed
- Anti-bacterial wipes can be used in the days prior to surgery
- Underlying illnesses such as diabetes needs to be carefully monitored and optimised
- Anaemia needs to be identified and treated
- Some medications such as steroids will increase the infection risk so need to be reviewed
Day of surgery
- I review your knee, shave any hair from the operative site and use a wash with a mixture of Chlorhexadine and Ethanol. The leg is then wrapped in a sterile drape so the next exposure will be in theatre, immediately prior to the start of procedure
- Myself and my assistant wear a sterile helmet and hood system so that everything that is directly in front of the surgical field is sterile. The system has a fan to circulate air which is only turned on once the gown and gloves are on and sealed. When used correctly, infection rates are reduced
Intra-operative measures
- Maximum single dose of broad-spectrum intravenous antibiotics is used with an effective duration of 24 hours
- No tourniquet is used for the majority of surgery (10-15minutes for cementation) to ensure all bleeding is caught early and there is no ischaemia of the tissues.
- The knee is draped so that only the surgical approach is visible and that is wrapped in an adhesive drape that releases an Iodine based antiseptic into the skin
- Surgery needs to be accurate and efficient to reduce surgical times
- Surgery needs to take great care of the soft tissues around the knee joint to allow healing without tissue injury or necrosis
- The capsule of the knee is sutured closed using a heavy barbed suture, this creates a water-tight seal so any bleeding is captured and doesn’t take the path of least resistance towards the dressing
- Tranexamic acid (TXA) prevents the normal breakdown of blood within the tissues and knee joint that has clotted and sealed off. It is used intravenously but importantly also intraarticularly after the knee capsular closure
- No drain is needed as all the bleeding has been stopped and the knee joint is now a closed system preventing an entry point for bacteria
- The skin is closed using a barbed suture and finally glue. Additional external skin closure such as steristrips aren’t necessary and can cause skin reactions
Post-operatively
- Post-op anaemia is prevented by minimising intra-operative bleeding and the TXA working within the sealed joint and systemically.
- The dressing is left intact for 12-14 days; using the intra-operative techniques dressing discharge is very rare.
- Any infections around the body such as urinary tract or chest are fully investigated and treated early with sensitive antibiotics
- Invasive dental treatment is covered with high dose broad-spectrum prophylactic antibiotics